Aging changes in the bones - muscles - joints
Information
Changes in posture and gait (walking pattern) are common with aging.
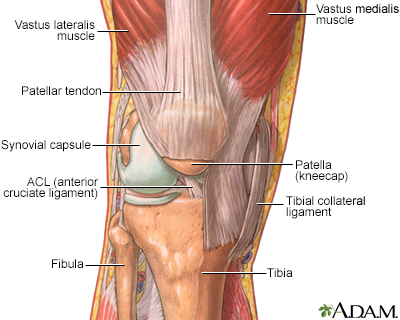
The skeleton provides support and structure to the body. Joints are the areas where bones come together. They allow the skeleton to be flexible for movement. In a joint, bones do not directly contact each other. Instead, they are cushioned by cartilage in the joint, synovial membranes around the joint, and fluid.
Video Transcript
Skeletal system components - Animation
The skeletal system consists of approximately 206 bones, providing the body with structure and support. Let’s take a tour of various components that form the skeletal system. Here’s the skull. It has 8 cranial bones that protect the brain. The facial skeleton has 14 bones that provide a framework for the eye sockets, jaws, and teeth. The facial bones provide the framework for the various structures of the face including the overlying muscles, fat and skin. The vertebral column is composed of 24 individual vertebrae, along with two sets of fused bones called the sacrum and coccyx. In addition to providing support for the trunk of the body, the vertebral column protects the spinal cord. All together, there are 7 cervical, or neck vertebrae; 12 thoracic, or upper back, vertebrae; and 5 lumbar, or lower back, vertebrae. The sacrum is composed of 5 fused bones, while the coccyx, or tailbone, is typically made up of 3 to 5 bones. 12 pairs of ribs form a protective cage for the heart, lungs, and other internal organs. The first 7 ribs are called true ribs because they attach to the breastbone, or sternum. Ribs 8 through 12 are called false ribs, because they either attach indirectly, or, as in the case with ribs 11 and 12, float and don’t attach to the sternum at all. Now let’s take a look at the pair of shoulder blades, or scapulae, and the collar bones, or clavicles. It is very important for the scapulae to be mobile, because they connect to the shoulder joint, which is the most movable joint in the body. The bones of the upper limb include the humerus, which connects the shoulder with the elbow, the ulna, the radius, the wrist bones or carpals, the hand bones or metacarpals, and the finger bones or phalanges. To complete our tour, let’s take a look at the pelvic girdle, knee, and foot. The pelvic girdle is formed by a pair of hip bones. Each hip bone is comprised of 3 fused bones, the ilium, ischium, and pubis. The pelvic girdle connects with the femur or thigh bone at the hip joint. The femur is the longest bone in the body and is important for bearing the body’s weight while standing. At the knee, the femur articulates with the tibia or shin bone. The fibula does not bear weight, but several muscles attach to it. The patella, or kneecap, is suspended within muscle tendons and glides over the femur and tibia when the knee bends. And last, but certainly not the least, are the feet. The foot bones, which include the tarsals, metatarsals, and phalanges, are organized into a series of arches that allow the feet to support the body’s weight.
Muscles provide the force and strength to move the body. Coordination is directed by the brain, but is affected by changes in the muscles and joints. Changes in the muscles, joints, and bones affect the posture and walk, and lead to weakness and slowed movement.
AGING CHANGES
People lose bone mass or density as they age, especially women after menopause. The bones lose calcium and other minerals.
Menopause
Menopause is the time in a woman's life when her periods (menstruation) stop. Most often, it is a natural, normal body change that occurs between ag...

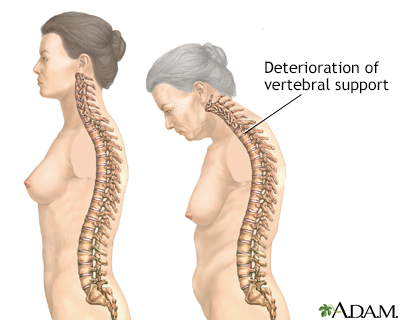
The spine is made up of bones called vertebrae. Between each bone is a gel-like cushion (called a disk). With aging, the middle of the body (trunk) becomes shorter as the disks gradually lose fluid and become thinner.
Vertebrae also lose some of their mineral content, making each bone thinner. The spinal column becomes curved and compressed (packed together). Bone spurs caused by aging and overall use of the spine may also form on the vertebrae.
The foot arches become less pronounced, contributing to a slight loss of height.
The long bones of the arms and legs are more brittle because of mineral loss, but they do not change length. This makes the arms and legs look longer when compared with the shortened trunk.
Long bones
Long bones are hard, dense bones that provide strength, structure, and mobility. The thigh bone (femur) is a long bone. A long bone has a shaft and...

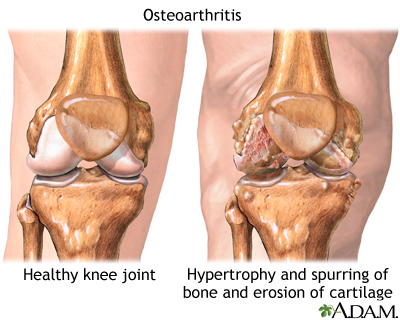
The joints become stiffer and less flexible. Fluid in the joints may decrease. The cartilage may begin to rub together and wear away. Minerals may deposit in and around some joints (calcification). This is common around the shoulder.
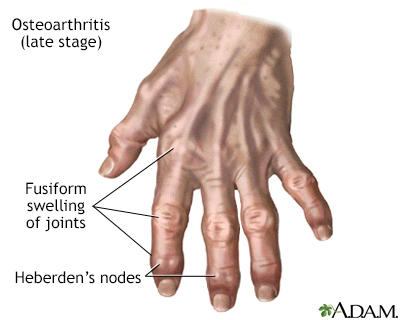
Hip and knee joints may begin to lose cartilage (degenerative changes). The finger joints lose cartilage and the bones thicken slightly. Finger joint changes, most often bony swelling called osteophytes, are more common in women. These changes may be inherited.
Lean body mass decreases. This decrease is partly caused by a loss of muscle tissue (atrophy). The speed and amount of muscle changes seem to be caused by genes. Muscle changes often begin in the 20s in men and in the 40s in women.
Atrophy
Muscle atrophy is the wasting (thinning) or loss of muscle tissue.

Lipofuscin (an age-related pigment) and fat are deposited in muscle tissue. The muscle fibers shrink. Muscle tissue is replaced more slowly. Lost muscle tissue may be replaced with a tough fibrous tissue. This is most noticeable in the hands, which may look thin and bony.
Muscles are less toned and less able to contract because of changes in the muscle tissue and normal aging changes in the nervous system. Muscles may become rigid with age and may lose tone, even with regular exercise.
Aging changes in the nervous system
The brain and nervous system are your body's central control center. They control your body's: MovementsSensesThoughts and memories They also help c...

EFFECT OF CHANGES
Bones become more brittle and may break more easily. Overall height decreases, mainly because the trunk and spine shorten.
Breakdown of the joints may lead to inflammation, pain, stiffness, and deformity. Joint changes affect almost all older people. These changes range from minor stiffness to severe arthritis.
Arthritis
Arthritis is inflammation or degeneration of one or more joints. A joint is the area where 2 bones meet. There are more than 100 different types of...

The posture may become more stooped (bent). The knees and hips may become more flexed. The neck may tilt, and the shoulders may narrow while the pelvis becomes wider.
Movement slows and may become limited. The walking pattern (gait) becomes slower and shorter. Walking may become unsteady, and there is less arm swinging. Older people get tired more easily and have less energy.
Strength and endurance change. Loss of muscle mass reduces strength.
COMMON PROBLEMS
Video Transcript
Osteoporosis - Animation
If you've ever watched an apartment or office building under construction, you've seen the metal scaffolding that keeps the building standing upright. Inside your body, bones are the scaffolding that keep you standing upright. As you get older, these supports can weaken. And if they get too weak, you could wind up with a fracture. Let's talk about the bone-thinning condition called osteoporosis. Your internal scaffolding was built when you were young. Calcium and other minerals helped strengthen your bones, provided that you got enough of them from your diet. As you get older, those minerals can start to leech out of your bones, leaving them brittle, fragile, and easily breakable, a condition known as osteoporosis. Women over 50 are especially at risk for osteoporosis because during menopause they lose estrogen, which helps to keep bones strong. The tricky part about osteoporosis is that it's hard to tell you have it. You may not have any symptoms until you've already fractured a bone. Getting a bone density scan, which measures bone thickness, is one way to find out whether you have osteoporosis so you can start treatment right away if you need it. To keep your bones strong, try to get at least 1,200 milligrams of calcium daily, paired with 1,000 international units of vitamin D, which helps your body absorb calcium. You can eat foods that are high in these nutrients, like frozen yogurt, salmon, and low-fat milk, or, if you're not a big fan of fish or dairy, you can take supplements. Weight bearing exercise is also your ally when it comes to strengthening bones. A combination of weight bearing exercises like walking or playing tennis, plus strength training and balance exercises will reduce your risk of getting a fracture if you fall. You will want to get at least thirty minutes of exercise three times a week to see the benefits. And, stop smoking. Cigarette smoke both accelerates bone loss and blocks treatments from being as affective. If you've been diagnosed with osteoporosis, your doctor may recommend drugs called bisphosphonates to prevent further bone damage. Other medicines, including calcitonin, parathyroid hormone, and raloxifene are also treatment options. Don't let bone loss get so far along that you could have a disabling fracture from a minor fall. Start strengthening your bones with diet and exercise while you're still young. As you get older, talk to your doctor about bone density scans, and ask whether you need to take medicine if you're at risk for, or are starting to show signs of osteoporosis. And if your bones aren't as strong as they used to be, avoid falls by wearing shoes that fit well, and clearing clutter on the floor before it can trip you up, and bring you down.
Osteoporosis is a common problem, especially for older women. Bones break more easily. Compression fractures of the vertebrae can cause pain and reduce mobility.
Osteoporosis
Osteoporosis is a disease in which bones become fragile and more likely to break (fracture).

Fractures
If more pressure is put on a bone than it can stand, it will split or break. A break of any size is called a fracture. If the broken bone punctures...

Muscle weakness contributes to fatigue, weakness, and reduced activity tolerance. Joint problems ranging from mild stiffness to debilitating arthritis (osteoarthritis) are very common.
Osteoarthritis
Osteoarthritis (OA) is the most common joint disorder. It is due to aging and wear and tear on a joint.

Video Transcript
Osteoarthritis - Animation
You used to take for granted that you could play a whole game of tennis or basketball without pain. But years of wear and tear have left their mark on your joints, and now your knees and hips hurt so much you can barely bend them. The pain you're feeling may be due to osteoarthritis, a problem many of us face as we get older. We all start out life with a thick layer of cartilage that cushions our joints in the space where the bones meet. That cartilage allows us to twist our legs to kick a soccer ball, or jump to shoot a basket. But years of running, jumping, and climbing stairs can wear out that cushion, leaving the bones rubbing painfully against each other. By age 70, just about everyone feels some pain and stiffness from osteoarthritis, especially when they get up in the morning or after they've overused the joint. You're more likely to have osteoarthritis if you're overweight. It's similar to what happens when you put extra weight on your bed. Eventually, you'll push on the springs so hard that you'll wear them out. The same is true for your joints. People who've had joint injuries or who have played certain sports are also more likely to get osteoarthritis. When you see your doctor about joint pain and stiffness, he'll check how well the joint moves and look for swelling around it. You probably won't be able to move the joint all the way. And when you do move it, it's likely to hurt and may make a cracking sound. An x-ray can confirm that you've lost cartilage around the joint. Unfortunately, there's no cure for osteoarthritis. But there are treatments to relieve the pain, including physical therapy, knee taping, special low load exercise programs, such as swimming, cycling, walking or stretching, and Tai chi in particular can be great for flexibility and strength. Over-the-counter medicines like topical Capsaicin, oral acetaminophen, aspirin, ibuprofen, and naproxen may help. Mud pack therapy may increase the benefit of whatever else you're doing. Your doctor may recommend getting a steroid injection into the joint to both relieve pain and reduce swelling. Another method, which injects artificial joint fluid into the knee, can relieve pain longer term, for up to six months. If the joint damage is really bad, you may need surgery to trim off damaged cartilage or to replace the affected joint in the knee, hip, shoulder, or elbow with an artificial joint. This is called joint replacement surgery, and is quite common for the both damaged hip and knee joints. Although it may hurt to move, staying active can help keep your joints healthy. Exercising can also help you lose the weight that's putting pressure on your sore joints. Ask your doctor to recommend a physical therapist, who can teach you exercises that strengthen the muscles supporting your joints. Osteoarthritis is different in everyone. Some people can get around fine with it while others have trouble doing even the simplest tasks, like bending down to get the morning paper. Before your joints get so stiff and painful that they limit your lifestyle, talk to your doctor about treatment and prevention options that can help you get around more like you used to.
The risk of injury increases because gait changes, instability, and loss of balance may lead to falls.
Gait changes
Walking abnormalities can be caused by many different types of problems. Problems with the joints, (such as arthritis), bones (such as deformities),...

Loss of balance
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...

Some older people have reduced reflexes. This is most often caused by changes in the muscles and tendons, rather than changes in the nerves. Decreased knee jerk or ankle jerk reflexes can occur. Some changes, such as a positive Babinski reflex, are not a normal part of aging.
Babinski reflex
Reflexes are responses that occur when the body receives a certain stimulus. The Babinski reflex occurs after the sole of the foot has been firmly s...
Read Article Now Book Mark ArticleInvoluntary movements (muscle tremors and fine movements called fasciculations) are more common in the older people. Older people who are not active may have weakness or abnormal sensations (paresthesias).
Fasciculations
Muscle twitches are fine movements of a small area of muscle.

Paresthesias
Numbness and tingling are abnormal sensations that can occur anywhere in your body, but they are often felt in your fingers, hands, feet, arms, or le...

People who are unable to move on their own, or who do not stretch their muscles with exercise, may get muscle contractures.
PREVENTION
Exercise is one of the best ways to slow or prevent problems with the muscles, joints, and bones. A moderate exercise program can help you maintain strength, balance, and flexibility. Exercise helps the bones stay strong.
Talk to your health care provider before starting a new exercise program.
It is important to eat a well-balanced diet with plenty of calcium. Women need to be particularly careful to get enough calcium and vitamin D as they age. Postmenopausal women and men over age 70 should take in 1,200 mg of calcium per day. Women and men over age 70 should get 800 international units (IU) of vitamin D daily. If you have osteoporosis, talk to your provider about prescription treatments.
RELATED TOPICS
-
Aging changes in body shape
Aging changes in body shape
Your body shape changes naturally as you age. You cannot avoid some of these changes, but your lifestyle choices may slow or speed the process. The ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Aging changes in hormone production
Aging changes in hormone production
The endocrine system is made up of organs and tissues that produce hormones. Hormones are natural chemicals produced in one location, released into ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Aging changes in organs, tissues, and cells
Aging changes in organs, tissues, and c...
All vital organs begin to lose some function as you age. Aging changes occur in all of the body's cells, tissues, and organs, and these changes affe...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Aging changes in the nervous system
Aging changes in the nervous system
The brain and nervous system are your body's central control center. They control your body's: MovementsSensesThoughts and memories They also help c...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Calcium in diet
Calcium in diet
Calcium is the most plentiful mineral found in the human body. The teeth and bones contain the most calcium. Nerve cells, body tissues, blood, and ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Osteoporosis
Osteoporosis
Osteoporosis is a disease in which bones become fragile and more likely to break (fracture).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Reviewed By
Frank D. Brodkey, MD, FCCM, Associate Professor, Section of Pulmonary and Critical Care Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 01/07/2025.
Di Cesare PE, Haudenschild DR, Abramson SB, Samuels J. Pathogenesis of osteoarthritis. In: Firestein GS, Budd RC, Gabriel SE, Koretzky GA, McInnes IB, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 104.
Gregson CL. Bone and joint aging. In: Fillit HM, Rockwood K, Young J, eds. Brocklehurst's Textbook of Geriatric Medicine and Gerontology. 8th ed. Philadelphia, PA: Elsevier; 2017:chap 20.
US Department of Health & Human Services. National Institutes of Health, Office of Dietary Supplements website. Vitamin D: fact sheet for health professionals. ods.od.nih.gov/factsheets/VitaminD-HealthProfessional. Updated July 26, 2024. Accessed January 7, 2025.
Walston JD. Common clinical sequelae of aging. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 24.
Weber TJ. Osteoporosis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 225.
Disclaimer





 All rights reserved.
All rights reserved.