Testicular torsion repair
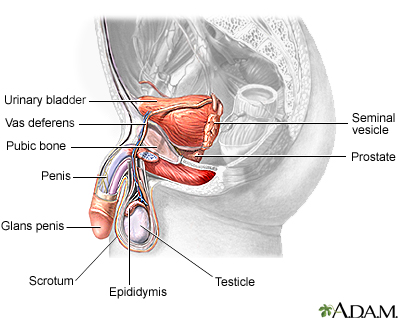
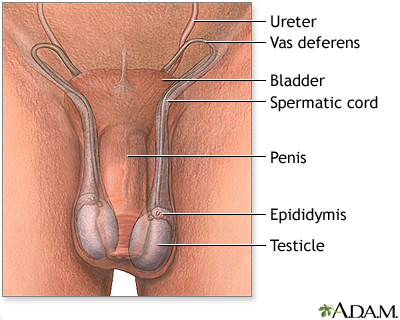
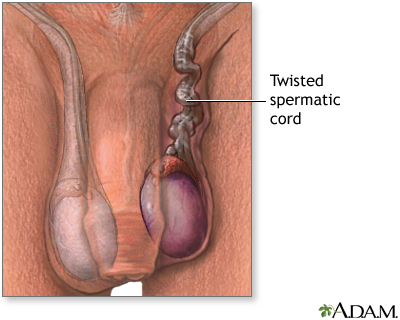
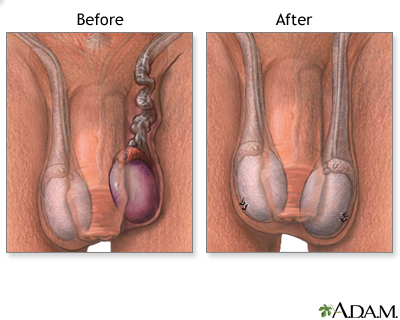
Testicular torsion repair is surgery to untangle or untwist a spermatic cord. The spermatic cord has a collection of blood vessels in the scrotum that lead to the testicles. Testicular torsion develops when the cord twists. This pulling and twisting blocks blood flow to the testicle.
Testicular torsion
Testicular torsion is twisting of the spermatic cord, which supports the testes in the scrotum. When this occurs, the blood supply is cut off to the...

Description
Most of the time, you will get general anesthesia for testicular torsion repair surgery. You will be asleep and pain-free.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep-like state so you do not feel pain during surgery. After you ...
Read Article Now Book Mark ArticleTo perform the procedure:
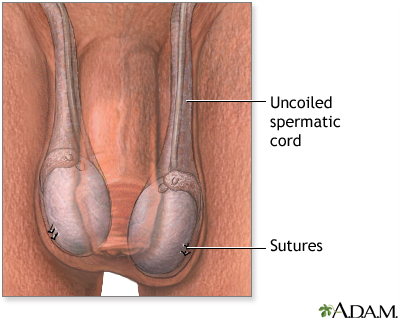
- The surgeon will make a cut in your scrotum to get to the twisted cord.
Scrotum
The scrotum is a part of a male's body that is located below the penis. The scrotum is the sac (pouch) that contains the testes, epididymis, and the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - The cord will be untwisted. The surgeon will then attach the testicle to the inside of your scrotum using stitches.
- The other testicle will be attached in the same way to prevent future problems.
Why the Procedure Is Performed
Testicular torsion is an emergency. In most cases, surgery is needed right away to relieve pain and swelling and to prevent the loss of the testicle. For the best results, surgery should be done within 4 hours after symptoms begin. By 12 hours, a testicle may become damaged so badly that it has to be removed.
Risks
Risks of this surgery are:
-
Bleeding
Bleeding
Bleeding is the loss of blood. Bleeding may be:Inside the body (internal)Outside the body (external)Bleeding may occur:Inside the body when blood le...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Infection
- Pain
- Wasting away of the testicle despite the return of blood flow
-
Infertility
Infertility
Infertility means you cannot get pregnant (conceive). There are 2 types of infertility:Primary infertility refers to couples who have not become preg...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Before the Procedure
Most of the time, this surgery is done as an emergency, so there is often too little time to have medical tests beforehand. You may have an imaging test (most often ultrasound) to check for blood flow and tissue death.
Tell your surgeon or nurse if:
- You are taking any medicines, including drugs, supplements, or herbs you bought without a prescription.
- You have been drinking a lot of alcohol, more than 1 or 2 drinks a day.
- If you have diabetes, heart disease, or other medical conditions.
Diabetes
Diabetes is a long-term (chronic) disease in which the body cannot regulate the amount of sugar in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHeart disease
Coronary heart disease is a narrowing of the blood vessels that supply blood and oxygen to the heart. Coronary heart disease (CHD) is also called co...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Most of the time, you will be given pain medicine and sent to a urologist for surgery as soon as possible.
After the Procedure
Following your surgery:
- Pain medicine, rest, and ice packs will relieve pain and swelling after surgery.
- Do not put the ice directly on your skin. Wrap it in a towel or cloth.
- Rest at home for several days. You may wear a scrotal support for a week after surgery.
- Avoid strenuous activity for 1 to 2 weeks. Slowly start doing your normal activities.
- You may resume sexual activity after about 4 to 6 weeks.
Outlook (Prognosis)
If surgery is done in time, you should have a complete recovery. When it is done within 4 hours after symptoms begin, the testicle can be saved most of the time.
If one testicle has to be removed, the remaining healthy testicle should provide enough hormones for normal male growth, sex life, and fertility.
Reviewed By
Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Di Carlo HN, Crigger CB. Disorders and anomalies of the scrotal contents. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 582.
Germann CA. Urologic disorders. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 85.
Palmer LS, Palmer JS. Management of abnormalities of the external genitalia in males. In: Domochowski RR, Kavoussi LR, Peters CA, et al, eds. Campbell-Walsh-Wein Urology. 13th ed. Philadelphia, PA: Elsevier; 2026:chap 55.
Park JH, Leitner DV, Elsamra SE. Evaluation of the urologic patient: history and physical examination. In: Dmochowski RR, Kavoussi LR, Peters CA, et al, eds. Campbell-Walsh-Wein Urology. 13th ed. Philadelphia, PA: Elsevier; 2026:chap 2.
Zee RS, Herndon CDA. Perinatal urology. In: Dmochowski RR, Kavoussi LR, Peters CA, et al, eds. Campbell-Walsh-Wein Urology. 13th ed. Philadelphia, PA: Elsevier; 2026:chap 34.
Disclaimer


 All rights reserved.
All rights reserved.