Arrhythmias
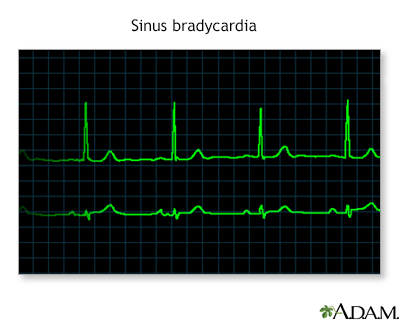
An arrhythmia is a disorder of the heart rate (pulse) or heart rhythm. The heart can beat too fast (tachycardia), too slow (bradycardia), or irregularly.
An arrhythmia can be harmless, a sign of other heart problems, or an immediate danger to your health.
Causes
Video Transcript
What makes your heart beat? - Animation
Let’s take a closer look inside the heart. The yellow objects are not nerves. They’re actually specialized cardiac muscle cells in the walls of the heart. Their job is to send signals to the rest of the heart muscle and cause a contraction. Together, this group of cells is called the Cardiac conduction system. The main components of the Cardiac conduction system are the SA node, AV node, Bundle of His, Bundle branches, and Purkinje fibers. Let’s follow a signal through the contraction process. The SA node starts the sequence by causing the atrial muscles to contract. That’s why doctors sometimes call it the anatomical pacemaker. From there, the signal travels to the AV node, through the Bundle of His, down the Bundle branches, and through the Purkinje fibers, causing the ventricles to contract. This signal creates an electrical current that can be seen on a graph called an Electrocardiogram, or EKG. Doctors us an EKG as a way of seeing how well the Cardiac conduction system works. Any changes to the EKG can mean serious problems.
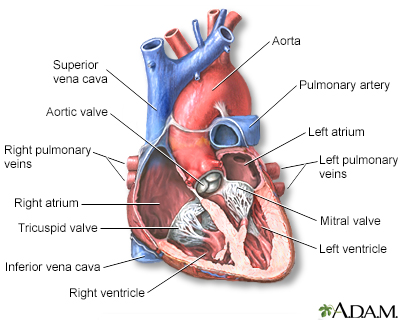
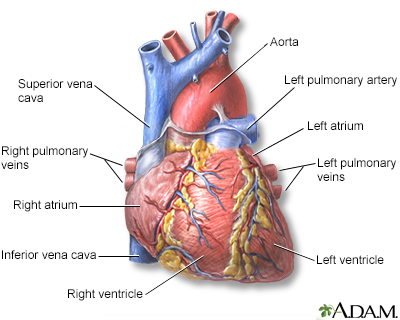
Normally, your heart works as a pump that brings blood to the lungs and the rest of the body.
To help this happen, your heart has an electrical system that makes sure it contracts (squeezes) in an orderly way.
- The electrical impulse that signals your heart to contract begins in an area of the heart called the sinoatrial node (also called the sinus node or SA node). This is your heart's natural pacemaker.
- The signal leaves the SA node and travels through the heart along a set electrical pathway.
- Different nerve messages signal your heart to beat slower or faster.
Video Transcript
Cardiac arrhythmia - conduction system overview - Animation
The heart is a muscular organ that beats in a rhythmic and coordinated fashion. This property of the heart is mainly due to the presence of a specialized in-house conduction system that generates electrical impulses in an orderly way. This system is known as the cardiac conduction system. The sequential, rhythmic, coordinated contractions of the heart are the result of the activity of the cardiac conduction system and the presence of gap junctions between adjacent cardiac muscle cells. The cardiac conduction system consists of specialized cardiac cells that are capable of generating and propagating electrical impulses throughout the heart muscle in a coordinated and sequential manner. The cardiac conduction system consists of the following structures: the sinoatrial (SA) node, the atrioventricular (AV) node, the atrioventricular (AV) bundle or the Bundle of His, the right and left bundle branches, and the Purkinje fibers.
Arrhythmias are caused by problems with the heart's electrical conduction system.
- Abnormal extra signals may occur.
- Electrical signals may be blocked or slowed.
- Electrical signals travel in new or different pathways through the heart.
Some common causes of abnormal heartbeats are:
- Abnormal levels of potassium, magnesium, or other substances in the body
- Heart attack, or a damaged heart muscle from a past heart attack
- Heart disease that is present at birth (congenital)
- Heart failure or an enlarged heart
- Overactive thyroid gland
Video Transcript
Arrhythmias - Animation
A change in the heart's normal electrical conduction system can result in an arrhythmia or irregular heartbeat. An arrhythmia can be an abnormally slow heartbeat, or an abnormally fast heartbeat. In some cases, it can be fatal.
Arrhythmias may also be caused by some substances or drugs, including:
- Alcohol or stimulant drugs
- Certain medicines
- Cigarette smoking (nicotine)
Some of the more common abnormal heart rhythms are:
-
Atrial fibrillation or flutter
Atrial fibrillation or flutter
Atrial fibrillation (AFib) and atrial flutter are common types of abnormal heart rhythms (arrhythmias) which affect the upper chambers (atria) of the...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Atrioventricular nodal reentry tachycardia (AVNRT)
- Heart block or atrioventricular block
-
Multifocal atrial tachycardia
Multifocal atrial tachycardia
Multifocal atrial tachycardia (MAT) is a rapid heart rate. It occurs when too many signals (electrical impulses) are sent from the upper heart (atri...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Paroxysmal supraventricular tachycardia
Paroxysmal supraventricular tachycardia
Paroxysmal supraventricular tachycardia (PSVT) is episodes of a rapid heart rate that start in a part of the heart above the ventricles. "Paroxysmal...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Sick sinus syndrome
Sick sinus syndrome
Normally, the heartbeat starts in an area in the top chambers of the heart (atria). This area is the heart's pacemaker. It is called the sinoatrial...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Ventricular fibrillation or ventricular tachycardia
Ventricular fibrillation
Ventricular fibrillation (VF) is a severely abnormal heart rhythm (arrhythmia) that is life threatening.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Wolff-Parkinson-White syndrome
Wolff-Parkinson-White syndrome
Wolff-Parkinson-White (WPW) syndrome is a condition in which there is an extra electrical pathway in the heart that leads to periods of rapid heart r...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Symptoms
When you have an arrhythmia, your heartbeat may be:
- Too slow (bradycardia)
- Too quick (tachycardia)
- Irregular, uneven, possibly with extra or skipped beats
An arrhythmia may be present all of the time or it may come and go. You may or may not feel symptoms when the arrhythmia is present. Or, you may only notice symptoms when you are more active.
Symptoms can be very mild, or they may be severe or even life threatening.
Common symptoms that may occur when the arrhythmia is present could include:
-
Chest pain
Chest pain
Chest pain is discomfort or pain that you feel anywhere along the front of your body between your neck and upper abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Fainting
Fainting
Fainting is a brief loss of consciousness due to a drop in blood flow to the brain. The episode most often lasts less than a couple of minutes and y...
Read Article Now Book Mark Article -
Lightheadedness, dizziness
Lightheadedness
Fainting is a brief loss of consciousness due to a drop in blood flow to the brain. The episode most often lasts less than a couple of minutes and y...
Read Article Now Book Mark ArticleDizziness
Dizziness is a term that is often used to describe 2 different symptoms: lightheadedness and vertigo. Lightheadedness is a feeling that you might fai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Paleness
Paleness
Paleness is an abnormal loss of color from normal skin or mucous membranes.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Palpitations (feeling your heart beat fast or irregularly)
-
Shortness of breath
Shortness of breath
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Sweating
Exams and Tests
The health care provider will listen to your heart with a stethoscope and feel your pulse. Your blood pressure may be low or normal or even high as a result of being uncomfortable.
An electrocardiogram (ECG) will be the first test done.
ECG
An electrocardiogram (ECG) is a test that records the electrical activity of the heart.

Video Transcript
Electrocardiogram - Animation
If your heart has been beating too fast, or you've been having chest pain, both you and your doctor will want to find out what's causing the problem so you can get it treated. One way to diagnose heart problems is with a test of the heart's electrical activity, called an electrocardiogram or ECG, or EKG for short. Your heart is controlled by an electrical system, much like the electricity that powers the lights and appliances in your home. Electrical signals make your heart contract so that it can pump blood out to your body. Heart disease, abnormal heart rhythms, and other heart problems can affect those signals. Using an ECG, your doctor can identify problems in your heart's electrical system and diagnose heart disease. So, how is an ECG done? First you'll lie down on a table. You'll have to lie very still while the test is done. Small patches, called electrodes, will be attached to several places on your arms, legs, and chest. The patches won't hurt, but some of the hair in those areas may be shaved so the patches will stick to your skin. The patches are then attached to a machine. You'll notice that when the machine is turned on, it produces wavy lines on a piece of paper. Those lines represent the electrical signals coming from your heart. If the test is normal, it should show that your heart is beating at an even rate of 60 to 100 beats per minute. Many different heart conditions can show up on an ECG, including a fast, slow, or abnormal heart rhythm, a heart defect, coronary artery disease, heart valve disease, or an enlarged heart. An abnormal ECG may also be a sign that you've had a heart attack in the past, or that you're at risk for one in the near future. If you're healthy and you don't have any family or personal history of heart disease, you don't need to have an ECG on a regular basis. But if you are having heart problems, your doctor may recommend getting this test. An ECG is pretty accurate at diagnosing many types of heart disease, although it doesn't always pick up every heart problem. You may have a perfectly normal ECG, yet still have a heart condition. If your test is normal but your doctor suspects that you have a heart problem, he may recommend that you have another ECG, or a different type of test to find out for sure.
Heart monitoring devices are often used to identify the rhythm problem, such as a:
-
Holter monitor (where you wear a device that records and stores your heart rhythm for 24 or more hours)
Holter monitor
A Holter monitor is a machine that continuously records the heart's rhythms. The monitor is worn for 24 to 48 hours during normal activity.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Event monitor or loop recorder (worn for 2 weeks or longer, where you record your heart rhythm when you feel an abnormal rhythm)
- Other long-term monitoring options
Video Transcript
Cardiac arrhythmia: Additional tests - Animation
Additional tests are sometimes used to evaluate patients with arrhythmia. The most common tests are long-term ECG recording, exercise testing, heart rate variability, electrophysiological studies, echocardiography and Doppler ultrasound tests, and blood tests. The choice of which test to use depends on the clinical circumstances.
An echocardiogram is sometimes ordered to examine the size or structure of your heart.
Echocardiogram
An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a s...

In selected cases, coronary angiography may be performed to see how blood flows through the arteries in your heart.
Coronary angiography
Coronary angiography is a procedure that uses a special dye (contrast material) and x-rays to see how blood flows through the arteries in your heart....

A special test, called an electrophysiology study (EPS), is sometimes done to take a closer look at the heart's electrical system.
Electrophysiology study
Intracardiac electrophysiology study (EPS) is a test to look at how well the heart's electrical signals are working. It is used to evaluate abnormal...

Video Transcript
Cardiac arrhythmia: Taking a medical history - Animation
In clinical practice, the first step in diagnosing a patient with suspected arrhythmia is history taking. The physician obtains the following pieces of information to help determine a diagnosis and guide further diagnostic testing: nature and mode of onset of symptoms and precipitating factors such as exercise and stress, mode of termination of symptoms, frequency, duration, and severity of symptoms, medication and dietary history, presence of systemic illnesses and known heart disease, and family history of arrhythmia.
Treatment
When an arrhythmia is serious, you may need urgent treatment to restore a normal rhythm. This may include:
- Electrical therapy (defibrillation or cardioversion)
- Implanting a short-term heart pacemaker
- Medicines given through a vein or by mouth
Sometimes, better treatment for your angina or heart failure will lower your chance of having an arrhythmia.
Medicines called anti-arrhythmic drugs may be used:
- To prevent an arrhythmia from happening again
- To keep your heart rate from becoming too fast or too slow
Some of these medicines can have side effects. Take them as prescribed by your provider. Do not stop taking the medicine or change the dose without first talking to your provider.
Other treatments to prevent or treat abnormal heart rhythms include:
-
Cardiac ablation, used to target areas in your heart that may be causing your heart rhythm problems
Cardiac ablation
Cardiac ablation is a procedure that is used to scar small areas in your heart that may be involved in your heart rhythm problems. This can prevent ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - An implantable cardioverter defibrillator, placed in people who are at high risk of sudden cardiac death
Implantable cardioverter defibrillator
An implantable cardioverter-defibrillator (ICD) is a device that detects a life-threatening, rapid heartbeat. This abnormal heartbeat is called an a...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Permanent pacemaker, a device that senses when your heart is beating too slowly. It sends a signal to your heart that makes your heart beat at the correct pace.
Pacemaker
A pacemaker is a small, battery-operated device. This device senses when your heart is beating too slowly. It sends a signal to your heart that mak...
Read Article Now Book Mark Article
Outlook (Prognosis)
The outcome depends on several factors:
- The kind of arrhythmia you have.
- Whether you have coronary artery disease, heart failure, or valvular heart disease.
Coronary artery disease
Coronary heart disease is a narrowing of the blood vessels that supply blood and oxygen to the heart. Coronary heart disease (CHD) is also called co...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHeart failure
Heart failure is a condition in which the heart is no longer able to pump oxygen-rich blood to the rest of the body efficiently. This causes symptom...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
When to Contact a Medical Professional
Contact your provider if:
- You develop any of the symptoms of a possible arrhythmia.
- You have been diagnosed with an arrhythmia and your symptoms worsen or do not improve with treatment.
Prevention
Taking steps to prevent coronary artery disease may reduce your chance of developing an arrhythmia.
Prevent coronary artery disease
Coronary heart disease (CHD) is a narrowing of the blood vessels that supply blood and oxygen to the heart. CHD is also called coronary artery disea...
Read Article Now Book Mark ArticleReviewed By
Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Executive summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2018;15(10):e190-e252. PMID: 29097320 pubmed.ncbi.nlm.nih.gov/29097320/.
Nattel S, Tomaselli GF. Mechanisms of cardiac arrhythmias. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 62.
Olgin JE. Approach to the patient with suspected arrhythmia. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 49.
Tracy CM, Epstein AE, Darbar D, et al. 2012 ACCF/AHA/HRS focused update of the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2012;60(14):1297-1313. PMID: 22975230 pubmed.ncbi.nlm.nih.gov/22975230/.
Disclaimer










 All rights reserved.
All rights reserved.