Proton pump inhibitors
Proton pump inhibitors (PPIs) are medicines that work by reducing the amount of stomach acid made by glands in the lining of your stomach.
How PPIs Help you
Proton pump inhibitors are used to:
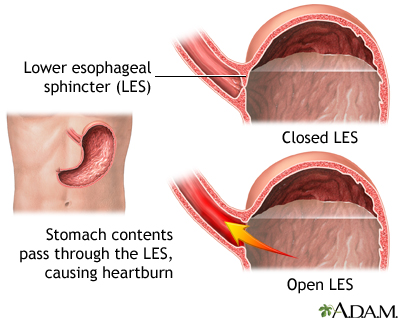
- Relieve symptoms of acid reflux, or gastroesophageal reflux disease (GERD). This is a condition in which food or liquid moves up from the stomach to the esophagus (the tube from the mouth to the stomach).
Gastroesophageal reflux disease
Gastroesophageal reflux disease (GERD) is a condition in which the stomach contents leak backward from the stomach into the esophagus (food pipe). F...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Treat a duodenal or stomach (gastric) ulcer.
Stomach (gastric) ulcer
A peptic ulcer is an open sore or raw area in the lining of the stomach (gastric ulcer) or in the first part of the small intestine (duodenal ulcer)....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Treat damage to the lower esophagus caused by acid reflux.
Types of PPIs
There are many names and brands of PPIs. Most work equally as well. Side effects may vary from drug to drug.
- Omeprazole (Prilosec), also available over-the-counter (without a prescription)
- Esomeprazole (Nexium), also available over-the-counter (without a prescription)
- Lansoprazole (Prevacid), also available over-the-counter (without a prescription)
- Rabeprazole (AcipHex)
- Pantoprazole (Protonix)
- Dexlansoprazole (Dexilant)
- Omeprazole with sodium bicarbonate (Zegerid OTC), available without a prescription
Taking Your PPIs
PPIs are taken by mouth. They are available as tablets or capsules. Commonly, these medicines are taken 30 minutes before the first meal of the day.
You can buy some brands of PPIs without a prescription. Talk to your health care provider if you find you have to take these medicines on most days. Some people who have acid reflux may need to take PPIs every day. Others may control symptoms with a PPI every other day.
If you have an ulcer, your provider may prescribe PPIs along with 2 or 3 other medicines for up to 2 weeks. Or your provider may ask you to take these medicines for 8 weeks.
If your provider prescribes these medicines for you:
- Take all of your medicines as you are told.
- Try to take them at the same time each day.
- It is best to take them before your first meal of the day.
- Do not stop taking your medicines without talking with your provider first. Follow up with your provider regularly.
- Plan ahead so that you do not run out of medicine. Make sure you have enough with you when you travel.
Side Effects
Side effects from PPIs are rare. You may have a headache, diarrhea, constipation, nausea, or itching. Ask your provider about possible concerns with long-term use, such as infections and bone fractures.
If you are breastfeeding or pregnant, talk to your provider before taking these medicines.
Tell your provider if you are also taking other medicines. PPIs may change the way certain medicines work, including some anti-seizure medicines and blood thinners such as warfarin or clopidogrel (Plavix).
When to Call the Doctor
Contact your provider if:
- You are having side effects from these medicines
- You are having other unusual symptoms
- Your symptoms are not improving
Reviewed By
Todd Eisner, MD, Private practice specializing in Gastroenterology in Boca Raton and Delray Beach, Florida at Gastroenterology Consultants of Boca Raton. Affiliate Assistant Professor, Florida Atlantic University School of Medicine. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Aronson JK. Proton pump inhibitors. In: Aronson JK, ed. Meyler's Side Effects of Drugs. 16th ed. Walthman, MA: Elsevier; 2016:1040-1045.
Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2022;117(1):27-56. PMID: 34807007 www.ncbi.nlm.nih.gov/pmc/articles/PMC8754510/.
Kuipers EJ, Blaser MJ. Acid peptic disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 125.
Richter JE, Vaezi MF. Gastroesophageal reflux disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 46.
Disclaimer


 All rights reserved.
All rights reserved.